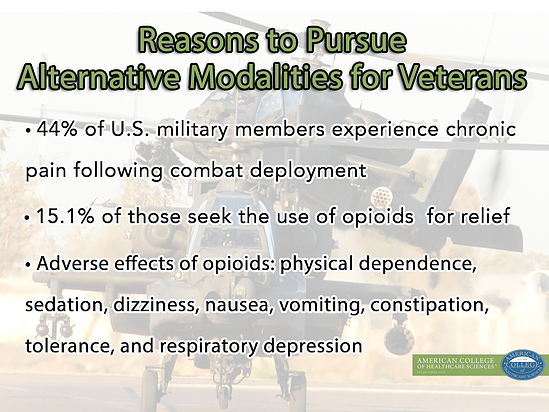
According to a study published in June, 44% of U.S. military members experience chronic pain following combat deployment. 15.1% of those seek the use of opioids[1] for relief.[2] This statistic is particularly disconcerting when it’s known that opioid use accompanies a slew of scary side effects such as “sedation, dizziness, nausea, vomiting, constipation, physical dependence, tolerance, and respiratory depression.” [3] Additionally, “opioids can be considered broad spectrum analgesic agents, affecting a wide number of organ systems and influencing a large number of body functions.”[4]
Isn’t it time we start seriously looking at alternative treatments for pain management for military servicemen, women, and veterans?
Here are just a few complementary alternative treatments that can be effective options for military members suffering from chronic pain post deployment:
Aromatherapy
Natural, plant-based essential oils have been shown to be highly effective in treating pain. One 2007 study examined the therapeutic effects of lavender essential oil on postoperative pain in patients recovering from laparoscopic gastric banding surgery, and “results suggest[ed] that lavender aromatherapy can be used to reduce the demand for opioids in the immediate postoperative period.”[5]
Given that the proper and safe use of essential oils has minimal to no adverse effects when used over time, aromatherapy is an ideal alternative to opioids. Not to mention, essential oils smell way better ; )
Another reason aromatherapy is an ideal option for veterans and returning military? It’s been shown to help soothe the symptoms of Post-traumatic Stress Disorder (PTSD). American College graduate and paramedic with the Alsip, IL Fire Department shared his incredible story of treating PTSD with aromatherapy (along with other CAM modalities) in a recent ACHS webinar.
ACHS President Dorene Petersen also wrote an article for Military Spouse that offers more insight into how aromatherapy is an effective alternative for PTSD: Aromatherapy Can Help PTSD.[6]
Herbal Medicine
Doesn’t a toasty cup of hot herbal tea or a soothing herbal compress sound better than popping a bunch of pills? Herbal remedies have been used to promote comfort and soothe pain for thousands of years.
Again, even though herbs for therapeutic purposes should be monitored by a trained health professional, the side effects are nowhere near as detrimental as the prolonged use of opioids.
Willow bark Salix alba (L.), turmeric Curcuma longa (L.), and cayenne Capsicum annuum (L.) are three herbs that should come to mind for pain.
Salicylic acid derived from willow bark was the main ingredient in modern day Aspirin, and willow bark has been used to treat chronic pain including back pain, rheumatic pain, toothaches, and headaches. Willow is powerful and should be used with caution as it can interact with medications as well as other herbs. Used under guidance from a qualified health professional, willow bark can be an effective alternative to opioids or other pharmaceuticals for chronic pain.[7]
Turmeric C. longa is another fantastic herbal example. A 2008 study on sciatic pain showed that turmeric (curcumin) “successfully prevented the development of neuropathic pain.”[8]
Cayenne pepper C. annuum also has a reputation as a soothing herb, and casaicin has even been used in topical preparations for rheumatoid arthritis, osteoarthritis, and fibromyalgia.[9] [10]
Sound interesting? Here is a cayenne liniment recipe you can try for yourself!
Soothing Cayenne Liniment
Cayenne Capsicum annuum: 1-2 tablespoons
Apple cider vinegar (or substitute with white vinegar): 1 cup
Boiling water: 1 cup
Steep all the ingredients for 15-30 minutes. Bottle and label. Rub onto painful areas after a hot bath or shower, and follow up with a rub with warmed olive oil.
Touch Therapies: Acupuncture and Massage
There are numerous studies showing the benefits of touch therapies such as acupuncture and massage in treating chronic pain.
Touch therapy is often used for a wide range of pain issues, such as migraines, carpal-tunnel syndrome, back pain, fibromyalgia… the list goes on!
A 2011 study (out of our home here in the Pacific Northwest!) showed that “massage therapy helped reduce pain and improve function more rapidly than usual medical care in people with chronic low-back pain.”[11] And according to the 2007 National Health Interview Survey, approximately 3.1 million Americans responded that they had used acupuncture within the last year. The NHIS also reported that pain—especially back pain—was the number one reason for using acupuncture.[12]
These studies are just the tip of the iceberg when it comes to showing how natural touch therapies can help sufferers of chronic pain with virtually no adverse effects.
What’s next?
It’s my belief that these alternative modalities are far better options for our returning soldiers than opioids (and/or other pain-relieving pharmaceuticals). As a holistic health educator, I am so encouraged to see ACHS students and graduates making positive strides in complementary alternative medicine for military members.
Learn More
ACHS student Brandie Lawrence conducted a thorough study on how CAM modalities impact the military family, and she presented her results in a Graduate Capstone webinar with ACHS: How CAM Impacts the Military Family. You can watch the video recording by clicking here or the image below.
What do you think about the rise of opioid use among members of the military? I’d love to see your thoughts in the comments below.
Disclosure of Material Connection: I am the CIO of American College of Healthcare Sciences, the Institution that publishes this blog. However, all opinions are my own. This blog may contain affiliate links. I am disclosing this in accordance with the Federal Trade Commission’s 16 CFR, Part 255: “Guides Concerning the Use of Endorsements and Testimonials in Advertising.”
This article is for informational purposes only. It is not intended to treat, diagnose, cure, or prevent disease. This article has not been reviewed by the FDA. Always consult with your primary care physician or naturopathic doctor before making any significant changes to your health and wellness routine.
Notes and References
[1] Opioids are psychoactive chemicals that works similarly to morphine or other opiates and used to reduce perception of pain.
[2] Toblin, R.L., Quartana, P.J., Riviere, L.A., Walper, K.C., & Hoge, C.W. (2014). Chronic pain and opioid use in U.S. soldiers After Combat Deployment. JAMA Intern Med, doi:10.1001/jamainternmed.2014.2726. Retrieved from http://archinte.jamanetwork.com/article.aspx?articleid=1885986
[3] Benyamin, R., Trescot, A.M., Datta, S., Buenaventura, R., Adlaka, R., Sehgal, N., Glaser, S,E,, Vallejo, R. (2008). Opioid complications and side effects. Pain Physician, S105-20.Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18443635
[4] Ibid.
[5] Kim J.T., Ren C.J., Fielding G.A., Pitti A., Kasumi T., Wajda M., Lebovits A., & Bekker A. (2007). Treatment with lavender aromatherapy in the post-anesthesia care unit reduces opioid requirements of morbidly obese patients undergoing laparoscopic adjustable gastric banding. Obes Surg. 17(7):920-5. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17894152
[6] This article was printed as being written by ACHS’s Marketing Director Kate Harmon. However, it was originally written by ACHS President Dorene Petersen.
[7] S. Chrubasik, O. Künzel, A. Model, C. Conradt and A. Black. Treatment of low back pain with a herbal or synthetic anti‐rheumatic: a randomized controlled study. Willow bark extract for low back pain. Rheumatology (Oxford). 2001 Dec;40(12):1388-93. Free full text available online here: http://rheumatology.oxfordjournals.org/content/40/12/1388.long
[8] Jeon, Y., Ha, J., Yeo, J., & Kim, Y. (2008, October 19). The effect of curcumin on neruropathic pain induced by chronic sciatic nerve ligation in rats. Anesthesiology. Retrieved from http://www.asaabstracts.com/strands/asaabstracts/abstract.htm;jsessionid=4C3B1ACE869E1F4AC0ECBD179C03A598?year=2008&index=3&absnum=991
[9]Covington TR, et al. Handbook of Nonprescription Drugs. 11th ed. Washington, DC: Am Pharmaceutical Assn, 1996. Mason L, Moore RA, Derry S, et al. Systematic review of topical capsaicin for the treatment of chronic pain. BMJ 2004;328:991.
[10] McCarty DJ, Csuka M, McCarthy G, et al. Treatment of pain due to fibromyalgia with topical capsaicin: A pilot study. Semin Arthr Rheum 1994;23:41-7.
[11] Cherkin DC, Sherman KJ, Kahn J, Wellman R, Cook AJ, Johnson E, et al. A Comparison of the Effects of 2 Types of Massage and Usual Care on Chronic Low Back Pain: A Randomized, Controlled Trial. Ann Intern Med. 2011;155:1-9. Retrieved from http://annals.org/article.aspx?articleid=747008
[12] National Center for Complementary Alternative Medicine. (2013, May 31). Acupuncture for Pain. nccam.nih.gov. Retrieved from http://nccam.nih.gov/health/acupuncture/acupuncture-for-pain.htm#use